Treatment
The cause of the infection determines the appropriate treatment. It may include oral or topical antibiotics and/or antifungal creams, antibacterial creams, or similar medications. A cream containing cortisone may also be used to relieve some of the irritation. If an allergic reaction is involved, an antihistamine may also be prescribed. For women who have irritation and inflammation caused by low levels of estrogen (postmenopausal), a topical estrogen cream might be prescribed.
Improved perineal hygiene is necessary to help healing and to prevent future reinfection for those whose infections are caused by bacteria normally found in stool. Sitz baths may be recommended. It is often helpful to allow more air to reach the genital area. Wearing cotton underwear (rather than nylon) or underwear that has a cotton lining in the crotch area allows greater air flow and decreases the amount of moisture in the area. Removing underwear at bedtime may also help.
Note: If a sexually transmitted disease is diagnosed, it is very important that your partner(s) receive treatment also, even if there are no symptoms. Many organisms don’t produce noticeable symptoms. Failure of the partner(s) to accept treatment can cause continual reinfection, which may eventually (if not taken care of) lead to more extensive problems, possibly limiting fertility and affecting overall health.
Prognosis (Expectations)
Proper treatment of an infection is usually very effective.
Complications
- Discomfort that does not go away
- Skin infection (from scratching)
- Complications due to the cause of the condition (such as gonorrhea and candida infection)
Calling Your Health Care Provider
Call your health care provider if vulvovaginitis symptoms are present or if known vulvovaginitis does not respond to treatment.
Pictures & Images
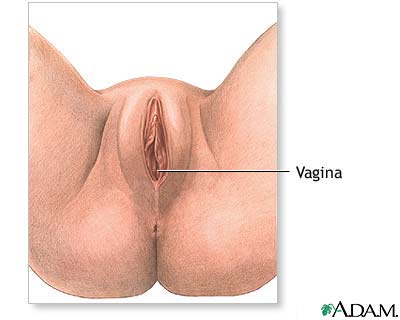
-
Vulvovaginitis: Overview, Causes
-
Vulvovaginitis: Symptoms & Signs, Diagnosis & Tests
-
Vulvovaginitis: Treatment
Review Date : 8/1/2008
Reviewed By : Linda Vorvick, MD, Seattle Site Coordinator, Lecturer, Pathophysiology, MEDEX Northwest Division of Physician Assistant Studies, University of Washington School of Medicine; and Susan Storck, MD, FACOG, Chief, Eastside Department of Obstetrics and Gynecology, Group Health Cooperative of Puget Sound, Redmond, Washington; Clinical Teaching Faculty, Department of Obstetrics and Gynecology, University of Washington School of Medicine. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc.
