Treatment
If the defect is small, no treatment is usually needed. However, the baby should be closely monitored by a health care provider to make sure that the hole eventually closes properly and signs of heart failure do not occur.
Babies with a large VSD who have symptoms related to heart failure may need medicine to control the symptoms and surgery to close the hole. Medications may include digitalis (digoxin) and diuretics.
If symptoms continue despite medication, surgery to close the defect with a Gore-tex patch is needed. Some VSDs can be closed with a special device during a cardiac catheterization, although this is infrequently done.
Surgery for a VSD with no symptoms is controversial. This should be carefully discussed with your health care provider.
Prognosis (Expectations)
Many small defects will close on their own. For those defects that do not spontaneously close, the outcome is good with surgical repair. Complications may result if a large defect is not treated.
Complications
- Heart failure
- Infective endocarditis (bacterial infection of the heart)
- Aortic insufficiency (leaking of the valve that separates the left ventricle from the aorta)
- Damage to the electrical conduction system of the heart during surgery (causing arrhythmias)
- Delayed growth and development (failure to thrive in infancy)
- Pulmonary hypertension (high blood pressure in the lungs) leading to failure of the right side of the heart
Calling Your Health Care Provider
Most often, this condition is diagnosed during routine examination of an infant. Call your infant’s health care provider if the baby seems to be having difficulty breathing, or if the baby seems to have an unusual number of respiratory infections.
Pictures & Images
Heart, section through the middle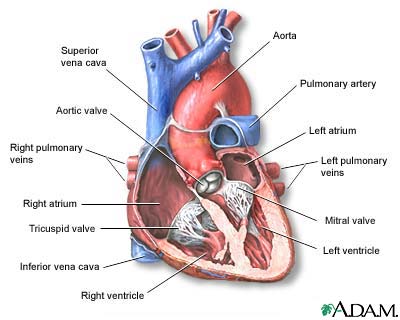
The interior of the heart is composed of valves, chambers, and associated vessels.
-
Ventricular septal defect: Overview, Causes
-
Ventricular septal defect: Symptoms & Signs, Diagnosis & Tests
-
Ventricular septal defect:Treatment
Review Date : 6/7/2008
Reviewed By : David C. Dugdale, III, MD, Professor of Medicine, Division of General Medicine, Department of Medicine, University of Washington School of Medicine; and Linda Vorvick, MD, Seattle Site Coordinator, Lecturer, Pathophysiology, MEDEX Northwest Division of Physician Assistant Studies, University of Washington School of Medicine. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc.
