Treatment
Treatment depends on various factors, including:
- Age
- General health
- Severity of symptoms
- Type of fibroids
- Whether you are pregnant
- If you want children in the future
Some women may just need pelvic exams or ultrasounds every once in a while to monitor the fibroid’s growth.
Treatment for the symptoms of fibroids may include:
- Birth control pills (oral contraceptives) to help control heavy periods
- Intrauterine devices (IUDs) that release the hormone progestin to help reduce heavy bleeding and pain
- Iron supplements to prevent or treat anemia due to heavy periods
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naprosyn for cramps or pain
Hormonal therapy (gonadotropin releasing hormone (GnRH) agonists or Depo Leuprolide injections) may be used to help shrink the fibroids. This therapy is used only for a short period of time, either before surgery to remove a fibroid or when a woman is expected to reach menopause soon. Side effects include hot flashes and vaginal dryness.
Surgery and procedures used to treat fibroids include:
- Hysteroscopic resection of fibroids: Women who have fibroids growing inside the uterine cavity may need this outpatient procedure. In this procedure, a small camera and instruments are inserted through the cervix into the uterus to remove the fibroid tumors.
- Uterine artery embolization: This procedure stops the blood supply to the fibroid, causing it to die and shrink. Uterine artery embolization is not used to treat large fibroids. Women who may want to become pregnant in the future should NOT have this procedure.
- Myomectomy: This surgery removes the fibroids. It is often the chosen treatment for women who want to have children, because it usually can preserve fertility. Another advantage of a myomectomy is that it controls pain or excessive bleeding that occurs in some women with uterine fibroids. More fibroids can develop after a myomectomy.
- Hysterectomy: This invasive surgery may be an option if medicines do not work and other surgeries and procedures are not an option.
Support Groups
National Uterine Fibroid Foundation – www.nuff.org
Prognosis (Expectations)
Some women with fibroids have no symptoms and may not need treatment.
During a pregnancy, existing fibroids may grow due to the increased blood flow and estrogen levels. The fibroids usually return to their original size after the baby is delivered.
Complications
Fibroids may cause pregnancy complications, although the risk is thought to be small:
- Most women are able to carry their babies to term, but some end up delivering prematurely because there is not enough room in the uterus.
- Some pregnant women with fibroids may need a cesarean section because fibroids can occasionally block the birth canal or cause the baby to be positioned wrong.
- Some pregnant women with fibroids have heavy bleeding immediately after giving birth.
Other complications of fibroids include:
- Severe pain or excessively heavy bleeding that may require emergency surgery
- A pedunculated fibroid can become twisted and cause a kink in the blood vessels feeding the tumor (this type of fibroid may need surgery)
- Anemia (which may be severe if the bleeding is very heavy)
- Urinary tract infections, if pressure from the fibroid prevents the bladder from fully emptying
- Cancerous changes called leiomyosarcoma (in rare cases)
- Infertility (rarely)
Calling Your Health Care Provider
Call your health care provider if:
- You have gradual changes in your menstrual pattern, including a heavier flow, increased cramping, or bleeding between periods
- Fullness or heaviness develops in your lower abdomen
Pictures & Images
Pelvic laparoscopy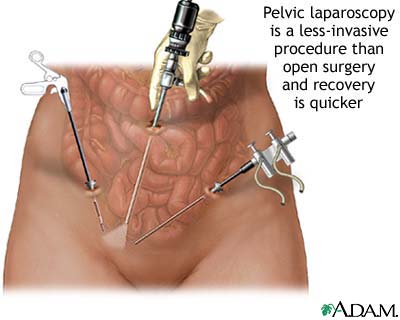
Laparoscopy is performed when less-invasive surgery is desired. It is also called “band-aid” surgery because only small incisions need to be made to accomodate the small surgical instruments that are used to view the abdominal contents and perform the surgery.
-
Uterine fibroids: Overview, Causes
-
Uterine fibroids: Symptoms & Signs, Diagnosis & Tests
-
Uterine fibroids: Treatment
Review Date : 9/2/2009
Reviewed By : Susan Storck, MD, FACOG, Chief, Eastside Department of Obstetrics and Gynecology, Group Health Cooperative of Puget Sound, Redmond, Washington; Clinical Teaching Faculty, Department of Obstetrics and Gynecology, University of Washington School of Medicine. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc.
![]()
