Treatment
The choice of treatment will depend on how severe the symptoms are, and how much they interfere with your lifestyle. There are three main treatment approaches for urge incontinence: medication, retraining, and surgery.
MEDICATION
If evidence of infection is found in a urine culture, your doctor will prescribe antibiotics.
Medications used to treat urge incontinence relax the involuntary bladder contractions and help improve bladder function. There are several types of medications that may be used alone or in combination:
- Anticholinergic medicines help relax the muscles of the bladder. They include oxybutynin (Oxytrol, Ditropan), tolterodine (Detrol), darifenacin (Enablex), trospium (Sanctura), solifenacin (Vesicare)
- These are the most commonly used medications for urge incontinence and are available in a once-a-day formula that makes dosing easy and effective.
- The most common side effects of these medicines are dry mouth and constipation. The medications cannot be used by patients with narrow angle glaucoma.
Flavoxate (Urispas) is an antispasmodic drug. However, studies have shown that it is not always effective at controlling symptoms of urge incontinence.
Tricyclic antidepressants (imipramine, doxepin) have also been used to treat urge incontinence because of their ability to “paralyze” the bladder smooth muscle. Possible side effects include:
- Blurred vision
- Dizziness
- Dry mouth
- Fatigue
- Insomnia
- Nausea
DIET
Drink plenty of water:
- Drinking enough water will help keep odors away.
- Drinking more water may even help reduce leakage.
Some experts recommend controlling fluid intake in addition to other therapies for managing urge incontinence. The goal of this program is to distribute fluids throughout the course of the day, so the bladder does not need to handle a large volume of urine at one time.
Do not drink large quantities of fluids with meals. Limit your intake to less than 8 ounces at one time. Sip small amounts of fluids between meals. Stop drinking fluids approximately 2 hours before bedtime.
It also may be helpful to eliminate foods that may irritate the bladder, such as:
- Caffeine
- Carbonated drinks
- Highly acidic foods such as citrus fruits and juices
- Spicy foods
BLADDER RETRAINING
Managing urge incontinence usually begins with a program of bladder retraining. Occasionally, electrical stimulation and biofeedback therapy may be used with bladder retraining.
A program of bladder retraining involves becoming aware of patterns of incontinence episodes. Then you relearn skills necessary for bladder storage and proper emptying.
Bladder retraining consists of developing a schedule of times when you should try to urinate. You try to consciously delay urination between these times.
One method is to force yourself to wait 1 to 1 1/2 hours between trips to the bathroom, despite any leakage or urge to urinate in between these times. As you become skilled at waiting, gradually increase the time intervals by 1/2 hour until you are urinating every 3 – 4 hours.
KEGEL EXERCISES
Pelvic muscle training exercises called Kegel exercises are primarily used to treat people with stress incontinence. However, these exercises may also be beneficial in relieving the symptoms of urge incontinence.
The principle behind Kegel exercises is to strengthen the muscles of the pelvic floor to improve the function of the urethral sphincter. The success of Kegel exercises depends on proper technique and sticking to a regular exercise program.
Another approach is to use vaginal cones to strengthen the muscles of the pelvic floor. A vaginal cone is a weighted device that is inserted into the vagina. The woman contracts the pelvic floor muscles in an effort to hold the device the place. The contraction should be held for up to 15 minutes and should be performed twice daily. Within 4 – 6 weeks, about 70% of women trying this method had some improvement in symptoms.
BIOFEEDBACK AND ELECTRICAL STIMULATION
Biofeedback and electrical stimulation can help identify the correct muscle group to work, to make sure you are performing Kegel exercises correctly.
Some therapists place a sensor in the vagina (for women) or the anus (for men) to assess contraction of the pelvic floor muscles. A monitor will display a graph showing which muscles are contracting and which are at rest. The therapist can help you identify the correct muscles for performing Kegel exercises.
Electrical stimulation involves using low-voltage electric current to stimulate the correct group of muscles. The current may be delivered using an anal or vaginal probe. The electrical stimulation therapy may be performed in the clinic or at home. Treatment sessions usually last 20 minutes and may be performed every 1 – 4 days.
SURGERY
Surgery can increase the storage ability of the bladder and decrease the pressure within the bladder. It is reserved for patients who are severely affected by their incontinence and have an unstable bladder (severe inappropriate contraction) and a poor ability to store urine.
Augmentation cystoplasty is the most often performed surgical procedure for severe urge incontinence. In this surgery, a segment of the bowel is added to the bladder to increase bladder size and allow the bladder to store more urine.
Possible complications are those of any major abdominal surgery, including:
- Blood clots
- Bowel obstruction
- Infection
- Pneumonia
There is a risk of developing abnormal tubelike passages (urinary fistulae) that result in abnormal urine drainage, urinary tract infection, and difficulty urinating. Augmentation cystoplasty is also linked to a slightly increased risk of developing tumors.
Sacral nerve stimulation is a newer surgical option that consists of an implanted unit that sends small electrical pulses to the sacral nerve. The electrical pulses can be adjusted to each patient’s symptoms.
ACTIVITY
People with urge incontinence may find it helpful to avoid activities that irritate the urethra and bladder, such as taking bubble baths or using harsh soaps in the genital area.
MONITORING
Urinary incontinence is a long-term (chronic) problem. Although you may be considered cured by treatment, you should continue to see your health care provider to evaluate the progress of your symptoms and monitor for possible treatment complications.
Prognosis (Expectations)
How well you do depends on your symptoms, an accurate diagnosis, and proper treatment. Many patients must try different therapies (some at the same time) to reduce symptoms.
Instant improvement is unusual. Perseverance and patience are usually required to see improvement. A small number of patients need surgery to control their symptoms.
Complications
Physical complications are rare. However, psychological and social problems may arise, particularly if you are unable to get to the bathroom when you feel the urge.
Calling Your Health Care Provider
Call your health care provider for an appointment if:
- Your symptoms are causing you problems
- You have pelvic discomfort or burning with urination
- Your symptoms occur dail
Pictures & Images
Female urinary tract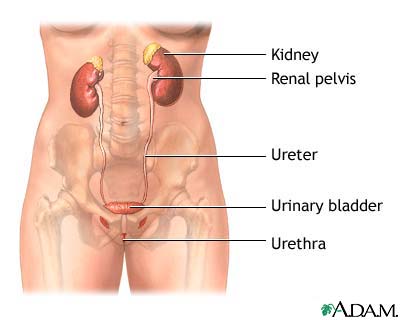
-
Urge incontinence: Overview, Causes
-
Urge incontinence: Symptoms & Signs, Diagnosis & Tests
-
Urge incontinence: Treatment
Review Date : 3/5/2010
Reviewed By : A.D.A.M. Editorial Team: David Zieve, MD, MHA, David R. Eltz. Previously reviewed by Louis S. Liou, MD, PhD, Assistant Professor of Urology, Department of Surgery, Boston University School of Medicine (8/30/2009).
![]()
